

Remote learning has revolutionized the educational landscape, offering aspiring medical coders a flexible and accessible pathway to enter this dynamic field. As healthcare systems grow ever more complex, the demand for skilled medical coders continues to rise. Remote learning provides an ideal solution for individuals seeking to embark on this career path while balancing other life commitments.
One of the most compelling benefits of remote learning for aspiring medical coders is the flexibility it offers. Traditional in-person classes often require students to adhere to rigid schedules, which can be challenging for those with work or family obligations. Remote learning platforms allow students to access coursework at their convenience, enabling them to study at their own pace and on their own time. Healthcare staffing agencies provide scalable solutions for growing facilities source medical staffing knowledge. This flexibility empowers learners to manage their education alongside other responsibilities, making it possible for more people to consider a career in medical coding.
Another significant advantage of remote learning is accessibility. Students from diverse geographical locations can enroll in top-tier programs without needing to relocate or commute long distances. This broadens opportunities for individuals who may not have access to quality educational institutions locally. Additionally, remote learning often provides access to a wide array of resources such as virtual libraries, online forums, and interactive tools that enhance the learning experience.
The cost-effectiveness of remote education also cannot be overlooked. Online courses often come at a fraction of the price of traditional classroom-based education due to reduced overhead costs. Furthermore, students save money on commuting and accommodation expenses associated with attending classes in person. These financial savings make pursuing a career in medical coding more attainable for many people.
Moreover, remote learning encourages self-discipline and independence-skills that are invaluable in any professional setting. Aspiring medical coders learn how to manage their time effectively and take ownership of their educational journey. This self-directed approach fosters critical thinking and problem-solving abilities that are essential in navigating the complexities of medical coding tasks.
Finally, remote learning allows aspiring coders to engage with diverse peer groups and instructors globally through virtual platforms. This interaction enriches the educational experience by exposing students to different perspectives and practices within the industry. Networking opportunities abound as well, providing connections that could prove beneficial when seeking employment after completing one's studies.
In conclusion, remote learning offers myriad benefits for aspiring medical coders by providing flexible scheduling options, increased accessibility, cost savings, development of essential professional skills, and expanded networking possibilities. As technology continues to advance and reshape how we learn, embracing these innovative educational models will undoubtedly play a crucial role in preparing future generations of skilled professionals ready to meet the demands of an evolving healthcare system.
In the ever-evolving landscape of healthcare, medical coding stands as a vital pillar, ensuring that patient information is accurately translated into standardized codes. These codes are essential for billing, statistical analysis, and maintaining comprehensive healthcare records. As the demand for skilled medical coders continues to rise, remote learning has emerged as a crucial avenue for acquiring key skills and knowledge in this field.
One of the most significant advantages of remote learning is its accessibility. Aspiring coders can access high-quality education from anywhere in the world without the constraints of geographical boundaries. This flexibility is particularly beneficial for individuals balancing work or personal commitments alongside their studies. Remote learning platforms offer a plethora of courses that cover fundamental concepts such as anatomy, physiology, and medical terminology-components that form the bedrock of proficient coding.
A critical skill set that remote learners must develop is an in-depth understanding of various coding systems such as ICD-10-CM (International Classification of Diseases), CPT (Current Procedural Terminology), and HCPCS (Healthcare Common Procedure Coding System). Mastery of these systems ensures accurate translation of complex medical procedures and diagnoses into alphanumeric codes. Remote courses often provide interactive modules and virtual simulations to reinforce this knowledge, offering practical experience akin to traditional classroom settings.
Moreover, remote learning emphasizes the importance of staying updated with regulatory changes and industry standards. The healthcare field is dynamic; thus, coders must continuously update their knowledge base to ensure compliance with current regulations. Many online programs incorporate regular updates and resources to help learners stay abreast of these changes.
Critical thinking and analytical skills are also paramount in medical coding. Coders must be adept at interpreting clinical documentation to assign appropriate codes accurately. Remote learning options encourage the development of these skills through case studies and problem-solving exercises that simulate real-world scenarios.
Another aspect where remote learning excels is fostering self-discipline and time management-traits indispensable for any successful coder working remotely or on-site. Online courses typically require learners to manage their own study schedules, providing an opportunity to hone these skills which are invaluable in professional settings.
Collaboration tools integrated into many online platforms also facilitate peer interaction through forums and group projects. This aspect mirrors workplace environments where communication with other healthcare professionals is essential for clarifying documentation or addressing discrepancies.
In conclusion, remote learning offers a rich tapestry of opportunities for aspiring medical coders to acquire essential skills and knowledge areas integral to their profession. With its inherent flexibility, focus on up-to-date content delivery, and emphasis on critical skill development, it equips learners with the tools necessary not only to enter but also excel in the field of medical coding amidst an ever-changing healthcare landscape.
In today's rapidly evolving educational landscape, the surge in remote learning options for medical coding has been remarkable. As healthcare systems become increasingly complex, the demand for skilled medical coders who can accurately translate patient information into standardized codes for billing and record-keeping purposes has grown significantly. This demand, coupled with technological advancements and a shift towards flexible learning environments, has led to the proliferation of online courses and platforms dedicated to training aspiring coders.
One of the most popular online platforms offering medical coding courses is Coursera. Known for its diverse course offerings across various disciplines, Coursera provides learners with access to programs developed by top universities and institutions worldwide. Courses such as "Medical Billing and Coding" introduce students to essential concepts in anatomy, physiology, medical terminology, and coding procedures. With video lectures, interactive quizzes, and peer-reviewed assignments, learners can gain comprehensive insights at their own pace.
Similarly, edX offers an array of courses tailored for those interested in mastering medical coding skills. Partnering with esteemed institutions like Harvard University and the University of Washington, edX provides high-quality content that combines theoretical knowledge with practical applications. Courses like "Health Informatics on FHIR" delve into advanced topics such as interoperability standards in healthcare data exchange while reinforcing fundamental coding principles.
For those seeking more specialized training focused solely on medical coding certifications, AAPC's online platform emerges as a leading choice. The American Academy of Professional Coders (AAPC) offers certification courses including Certified Professional Coder (CPC), Certified Outpatient Coder (COC), and Certified Inpatient Coder (CIC). These programs are designed to equip learners with industry-standard skills necessary for accurate code assignment across various clinical settings. Students benefit from expert-led webinars, interactive forums for discussion among peers globally situated professionals -all accessible remotely via AAPC's user-friendly portal.
Another noteworthy mention is AHIMA's Virtual Lab which enables students enrolled through academic partners access hands-on experience using real-world health information management software applications utilized within healthcare facilities today; it serves not only students but also instructors aiming at enhancing curricula aligned closely current industry practices ultimately preparing future workforce effectively capable handling challenges faced modern-day HIM departments nationwide
The flexibility these platforms offer allows working professionals or individuals juggling multiple commitments simultaneously pursue education without compromising existing responsibilities-a crucial advantage making remote options highly attractive especially considering dynamic nature both personal professional lives present-day society demands adaptability ever-increasing rate
Moreover cost-effectiveness associated pursuing virtual education should not be overlooked traditional classroom-based instruction often entails expenses related commuting housing textbooks whereas many digital resources freely available open-source format reducing financial burden considerably democratizing access quality education ensuring greater inclusivity historically marginalized communities underrepresented sectors workforce alike
In conclusion expanding universe opportunity afforded burgeoning field underscores vital role innovative solutions play shaping tomorrow's leaders experts committed advancing global health initiatives leveraging technology maximize potential positively impact countless lives around world Through continued investment development robust engaging accessible e-learning modalities future bright indeed!

In today's rapidly evolving healthcare industry, the role of medical coders has become increasingly vital. These professionals are responsible for translating patient diagnoses, treatments, and procedures into standardized codes used for billing and record-keeping. As the demand for skilled coders rises, certification programs have emerged as a crucial component in ensuring that individuals possess the necessary knowledge and competencies. With the advent of remote learning options, aspiring medical coders now have unprecedented access to quality education and certification opportunities from virtually anywhere.
Certification programs serve as a benchmark for proficiency in medical coding. They provide structured curricula that cover essential topics such as anatomy, physiology, medical terminology, and coding guidelines. Moreover, these programs often culminate in an examination that tests a candidate's ability to apply this knowledge effectively. Employers tend to favor certified coders because these credentials signify a commitment to professionalism and an assurance of competence. Furthermore, certified coders often enjoy enhanced job prospects and potential for higher salaries compared to their non-certified counterparts.
Remote learning has revolutionized how individuals can pursue certification in medical coding. Online platforms offer flexibility that traditional classroom settings cannot match. Students can tailor their study schedules around personal commitments or work obligations, making it feasible for more people to enter the field of medical coding without significant disruption to their daily lives. This accessibility is particularly beneficial for those living in remote areas who might otherwise lack local educational resources.
The interactive nature of many online programs also enhances learning experiences by providing engaging content through multimedia presentations, virtual labs, and discussion forums where students can collaborate with peers across the globe. Additionally, remote learning courses often incorporate real-world scenarios into their modules, allowing students to gain practical insights into everyday challenges faced by professional coders.
Despite its advantages, remote learning does require self-discipline and motivation from students due to its inherently independent nature. However, reputable online certification programs are designed with support systems such as dedicated instructors and academic advisors who guide learners throughout their courses.
In conclusion, certification programs play an indispensable role in preparing competent medical coders ready to meet industry demands. The rise of remote learning options further democratizes access to these vital credentials by removing geographical barriers and offering flexible study solutions tailored to individual needs. As healthcare continues its trajectory towards greater reliance on technology and data-driven decision-making processes, certified medical coders will remain integral contributors within this dynamic landscape-an outcome made more achievable through comprehensive online education pathways.
In recent years, remote learning has revolutionized the way education is delivered across various fields, including medical coding. As healthcare systems worldwide increasingly rely on digital solutions, the demand for skilled medical coders continues to grow. For those considering a career in this field, remote medical coding education offers an accessible and flexible pathway to success. However, navigating this virtual landscape requires specific strategies to maximize learning outcomes and ensure professional readiness.
One of the most critical tips for succeeding in remote medical coding education is developing a structured study routine. The flexibility of online courses can be both a blessing and a challenge; without the traditional framework of in-person classes, students must be proactive in managing their time effectively. Establishing a consistent daily or weekly schedule that allocates dedicated study hours can help maintain discipline and prevent procrastination. Setting specific goals for each study session can further enhance focus and productivity.
Additionally, leveraging available technology is crucial in remote learning environments. Medical coding programs often provide various digital tools designed to facilitate understanding complex concepts. Students should take full advantage of these resources, which may include interactive modules, video lectures, and virtual simulations that mimic real-world coding scenarios. Familiarity with essential software used in the industry, such as electronic health records (EHR) systems and coding databases like ICD-10-CM or CPT codes, will also serve as an invaluable asset during training.
Active engagement with instructors and peers is another key factor for success. Online forums, discussion boards, and group projects offer opportunities to collaborate and learn from others' experiences. Participating actively in these platforms not only deepens one's understanding but also builds a support network that can be instrumental throughout the course duration-and beyond graduation when seeking employment opportunities or career advice.
Furthermore, students should seek out additional resources beyond their formal coursework to supplement their learning. This might involve reading current industry publications or joining professional organizations such as the American Academy of Professional Coders (AAPC). These activities keep learners informed about emerging trends and best practices within the medical coding field while broadening their knowledge base.
Finally, it's important for students to cultivate self-motivation and resilience throughout their educational journey. Remote learning might present unique challenges-such as feelings of isolation or technical difficulties-but maintaining a positive attitude and being adaptable will help overcome these obstacles. Celebrating small achievements along the way can boost morale and reinforce commitment toward achieving long-term career objectives.
In summary, success in remote medical coding education hinges on establishing effective study habits, utilizing technological tools wisely, engaging actively with educational communities, seeking external knowledge sources diligently-and perhaps most importantly-nurturing personal drive amid challenges inherent to online learning environments. By embracing these strategies wholeheartedly from day one onwards-aspiring coders are well-positioned not only succeed academically but thrive professionally within this dynamic healthcare niche poised at intersecting paths between medicine technology data analytics alike!
Remote learning has become an indispensable tool for education in the digital age, offering flexibility and accessibility that traditional classrooms cannot. This shift is particularly significant in fields like medical coding, where professionals need to stay updated with the ever-evolving healthcare industry standards. However, remote learning in medical coding presents its own set of challenges that learners must overcome to succeed.
One of the primary challenges is the complexity of the subject matter itself. Medical coding involves understanding intricate details about healthcare procedures, diagnoses, and billing processes. Without a physical classroom environment where students can easily ask questions and receive immediate feedback, learners may struggle to grasp these complex concepts. To overcome this challenge, interactive online platforms that provide real-time support through discussion forums or virtual office hours can be highly beneficial. Additionally, incorporating multimedia resources such as video lectures and interactive simulations can help demystify complicated topics.
Another significant hurdle is maintaining motivation and discipline in a self-paced learning environment. Unlike traditional settings where peer interaction acts as a motivator, remote learners often find themselves isolated, which can lead to procrastination or disengagement from the course material. To address this issue, creating structured schedules and setting specific goals can keep learners on track. Furthermore, joining online study groups or forums can foster a sense of community and accountability among peers.
Technical issues also pose a considerable challenge in remote learning for medical coders. Reliable internet access and up-to-date technology are prerequisites for participating effectively in online courses. Technical difficulties such as connectivity problems or software incompatibility can disrupt learning experiences significantly. Institutions providing remote education should ensure that their platforms are user-friendly and offer technical support services to assist students facing these issues.
Lastly, there is the challenge of assessment integrity in remote learning environments. Ensuring that students are evaluated fairly while preventing dishonest practices like plagiarism requires careful planning by educators. Utilizing diverse forms of assessment such as open-book exams, practical assignments, and regular quizzes can help maintain academic integrity.
In conclusion, while remote learning offers unparalleled opportunities for aspiring medical coders by providing flexible learning pathways, it also comes with distinct challenges that need strategic solutions. By leveraging technology effectively-through interactive platforms and supportive communities-students can navigate these hurdles successfully and emerge competent in their field even without traditional classroom experiences. As both educational institutions and learners adapt to this new normal in education delivery methods more innovative approaches will undoubtedly continue emerging making remote learning increasingly effective over time.

A hospital is a healthcare institution providing patient treatment with specialized health science and auxiliary healthcare staff and medical equipment.[1] The best-known type of hospital is the general hospital, which typically has an emergency department to treat urgent health problems ranging from fire and accident victims to a sudden illness. A district hospital typically is the major health care facility in its region, with many beds for intensive care and additional beds for patients who need long-term care.
Specialized hospitals include trauma centers, rehabilitation hospitals, children's hospitals, geriatric hospitals, and hospitals for specific medical needs, such as psychiatric hospitals for psychiatric treatment and other disease-specific categories. Specialized hospitals can help reduce health care costs compared to general hospitals.[2] Hospitals are classified as general, specialty, or government depending on the sources of income received.
A teaching hospital combines assistance to people with teaching to health science students and auxiliary healthcare students. A health science facility smaller than a hospital is generally called a clinic. Hospitals have a range of departments (e.g. surgery and urgent care) and specialist units such as cardiology. Some hospitals have outpatient departments and some have chronic treatment units. Common support units include a pharmacy, pathology, and radiology.
Hospitals are typically funded by public funding, health organizations (for-profit or nonprofit), health insurance companies, or charities, including direct charitable donations. Historically, hospitals were often founded and funded by religious orders, or by charitable individuals and leaders.[3]
Hospitals are currently staffed by professional physicians, surgeons, nurses, and allied health practitioners. In the past, however, this work was usually performed by the members of founding religious orders or by volunteers. However, there are various Catholic religious orders, such as the Alexians and the Bon Secours Sisters that still focus on hospital ministry in the late 1990s, as well as several other Christian denominations, including the Methodists and Lutherans, which run hospitals.[4] In accordance with the original meaning of the word, hospitals were original "places of hospitality", and this meaning is still preserved in the names of some institutions such as the Royal Hospital Chelsea, established in 1681 as a retirement and nursing home for veteran soldiers.
During the Middle Ages, hospitals served different functions from modern institutions in that they were almshouses for the poor, hostels for pilgrims, or hospital schools. The word "hospital" comes from the Latin hospes, signifying a stranger or foreigner, hence a guest. Another noun derived from this, hospitium came to signify hospitality, that is the relation between guest and shelterer, hospitality, friendliness, and hospitable reception. By metonymy, the Latin word then came to mean a guest-chamber, guest's lodging, an inn.[5] Hospes is thus the root for the English words host (where the p was dropped for convenience of pronunciation) hospitality, hospice, hostel, and hotel. The latter modern word derives from Latin via the Old French romance word hostel, which developed a silent s, which letter was eventually removed from the word, the loss of which is signified by a circumflex in the modern French word hôtel. The German word Spital shares similar roots.
Some patients go to a hospital just for diagnosis, treatment, or therapy and then leave ("outpatients") without staying overnight; while others are "admitted" and stay overnight or for several days or weeks or months ("inpatients"). Hospitals are usually distinguished from other types of medical facilities by their ability to admit and care for inpatients whilst the others, which are smaller, are often described as clinics.
The best-known type of hospital is the general hospital, also known as an acute-care hospital. These facilities handle many kinds of disease and injury, and normally have an emergency department (sometimes known as "accident & emergency") or trauma center to deal with immediate and urgent threats to health. Larger cities may have several hospitals of varying sizes and facilities. Some hospitals, especially in the United States and Canada, have their own ambulance service.
A district hospital typically is the major health care facility in its region, with large numbers of beds for intensive care, critical care, and long-term care.
In California, "district hospital" refers specifically to a class of healthcare facility created shortly after World War II to address a shortage of hospital beds in many local communities.[6][7] Even today, district hospitals are the sole public hospitals in 19 of California's counties,[6] and are the sole locally accessible hospital within nine additional counties in which one or more other hospitals are present at a substantial distance from a local community.[6] Twenty-eight of California's rural hospitals and 20 of its critical-access hospitals are district hospitals.[7] They are formed by local municipalities, have boards that are individually elected by their local communities, and exist to serve local needs.[6][7] They are a particularly important provider of healthcare to uninsured patients and patients with Medi-Cal (which is California's Medicaid program, serving low-income persons, some senior citizens, persons with disabilities, children in foster care, and pregnant women).[6][7] In 2012, district hospitals provided $54 million in uncompensated care in California.[7]



A specialty hospital is primarily and exclusively dedicated to one or a few related medical specialties.[8] Subtypes include rehabilitation hospitals, children's hospitals, seniors' (geriatric) hospitals, long-term acute care facilities, and hospitals for dealing with specific medical needs such as psychiatric problems (see psychiatric hospital), cancer treatment, certain disease categories such as cardiac, oncology, or orthopedic problems, and so forth.
In Germany, specialised hospitals are called Fachkrankenhaus; an example is Fachkrankenhaus Coswig (thoracic surgery). In India, specialty hospitals are known as super-specialty hospitals and are distinguished from multispecialty hospitals which are composed of several specialties.[citation needed]
Specialised hospitals can help reduce health care costs compared to general hospitals. For example, Narayana Health's cardiac unit in Bangalore specialises in cardiac surgery and allows for a significantly greater number of patients. It has 3,000 beds and performs 3,000 paediatric cardiac operations annually, the largest number in the world for such a facility.[2][9] Surgeons are paid on a fixed salary instead of per operation, thus when the number of procedures increases, the hospital is able to take advantage of economies of scale and reduce its cost per procedure.[9] Each specialist may also become more efficient by working on one procedure like a production line.[2]
A teaching hospital delivers healthcare to patients as well as training to prospective medical professionals such as medical students and student nurses. It may be linked to a medical school or nursing school, and may be involved in medical research. Students may also observe clinical work in the hospital.[10]
Clinics generally provide only outpatient services, but some may have a few inpatient beds and a limited range of services that may otherwise be found in typical hospitals.
A hospital contains one or more wards that house hospital beds for inpatients. It may also have acute services such as an emergency department, operating theatre, and intensive care unit, as well as a range of medical specialty departments. A well-equipped hospital may be classified as a trauma center. They may also have other services such as a hospital pharmacy, radiology, pathology, and medical laboratories. Some hospitals have outpatient departments such as behavioral health services, dentistry, and rehabilitation services.
A hospital may also have a department of nursing, headed by a chief nursing officer or director of nursing. This department is responsible for the administration of professional nursing practice, research, and policy for the hospital.
Many units have both a nursing and a medical director that serve as administrators for their respective disciplines within that unit. For example, within an intensive care nursery, a medical director is responsible for physicians and medical care, while the nursing manager is responsible for all the nurses and nursing care.
Support units may include a medical records department, release of information department, technical support, clinical engineering, facilities management, plant operations, dining services, and security departments.
The COVID-19 pandemic stimulated the development of virtual wards across the British NHS. Patients are managed at home, monitoring their own oxygen levels using an oxygen saturation probe if necessary and supported by telephone. West Hertfordshire Hospitals NHS Trust managed around 1200 patients at home between March and June 2020 and planned to continue the system after COVID-19, initially for respiratory patients.[12] Mersey Care NHS Foundation Trust started a COVID Oximetry@Home service in April 2020. This enables them to monitor more than 5000 patients a day in their own homes. The technology allows nurses, carers, or patients to record and monitor vital signs such as blood oxygen levels.[13]
In early India, Fa Xian, a Chinese Buddhist monk who travelled across India c. AD 400, recorded examples of healing institutions.[14] According to the Mahavamsa, the ancient chronicle of Sinhalese royalty, written in the sixth century AD, King Pandukabhaya of Sri Lanka (r. 437–367 BC) had lying-in-homes and hospitals (Sivikasotthi-Sala).[15] A hospital and medical training center also existed at Gundeshapur, a major city in southwest of the Sassanid Persian Empire founded in AD 271 by Shapur I.[16] In ancient Greece, temples dedicated to the healer-god Asclepius, known as Asclepeion functioned as centers of medical advice, prognosis, and healing.[17] The Asclepeia spread to the Roman Empire. While public healthcare was non-existent in the Roman Empire, military hospitals called valetudinaria did exist stationed in military barracks and would serve the soldiers and slaves within the fort.[18] Evidence exists that some civilian hospitals, while unavailable to the Roman population, were occasionally privately built in extremely wealthy Roman households located in the countryside for that family, although this practice seems to have ended in 80 AD.[19]
The declaration of Christianity as an accepted religion in the Roman Empire drove an expansion of the provision of care.[20] Following the First Council of Nicaea in AD 325 construction of a hospital in every cathedral town was begun, including among the earliest hospitals by Saint Sampson in Constantinople and by Basil, bishop of Caesarea in modern-day Turkey.[21] By the twelfth century, Constantinople had two well-organised hospitals, staffed by doctors who were both male and female. Facilities included systematic treatment procedures and specialised wards for various diseases.[22]
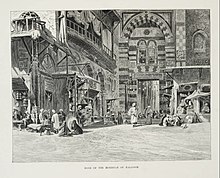
The earliest general hospital in the Islamic world was built in 805 in Baghdad by Harun Al-Rashid.[23][24] By the 10th century, Baghdad had five more hospitals, while Damascus had six hospitals by the 15th century, and Córdoba alone had 50 major hospitals, many exclusively for the military, by the end of the 15th century.[25] The Islamic bimaristan served as a center of medical treatment, as well nursing home and lunatic asylum. It typically treated the poor, as the rich would have been treated in their own homes.[26] Hospitals in this era were the first to require medical licenses for doctors, and compensation for negligence could be made.[27][28] Hospitals were forbidden by law to turn away patients who were unable to pay.[29] These hospitals were financially supported by waqfs, as well as state funds.[25]
In India, public hospitals existed at least since the reign of Firuz Shah Tughlaq in the 14th century. The Mughal emperor Jahangir in the 17th century established hospitals in large cities at government expense with records showing salaries and grants for medicine being paid for by the government.[30]
In China, during the Song dynasty, the state began to take on social welfare functions previously provided by Buddhist monasteries and instituted public hospitals, hospices and dispensaries.[31]
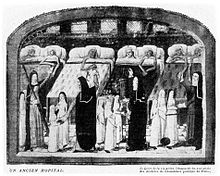
In Europe the medieval concept of Christian care evolved during the 16th and 17th centuries into a secular one. In England, after the dissolution of the monasteries in 1540 by King Henry VIII, the church abruptly ceased to be the supporter of hospitals, and only by direct petition from the citizens of London, were the hospitals St Bartholomew's, St Thomas's and St Mary of Bethlehem's (Bedlam) endowed directly by the crown; this was the first instance of secular support being provided for medical institutions.
In 1682, Charles II founded the Royal Hospital Chelsea as a retirement home for old soldiers known as Chelsea Pensioners, an instance of the use of the word "hospital" to mean an almshouse.[32] Ten years later, Mary II founded the Royal Hospital for Seamen, Greenwich, with the same purpose.[33]



The voluntary hospital movement began in the early 18th century, with hospitals being founded in London by the 1720s, including Westminster Hospital (1719) promoted by the private bank C. Hoare & Co and Guy's Hospital (1724) funded from the bequest of the wealthy merchant, Thomas Guy.
Other hospitals sprang up in London and other British cities over the century, many paid for by private subscriptions. St Bartholomew's in London was rebuilt from 1730 to 1759,[38] and the London Hospital, Whitechapel, opened in 1752.
These hospitals represented a turning point in the function of the institution; they began to evolve from being basic places of care for the sick to becoming centers of medical innovation and discovery and the principal place for the education and training of prospective practitioners. Some of the era's greatest surgeons and doctors worked and passed on their knowledge at the hospitals.[39] They also changed from being mere homes of refuge to being complex institutions for the provision and advancement of medicine and care for sick. The Charité was founded in Berlin in 1710 by King Frederick I of Prussia as a response to an outbreak of plague.
Voluntary hospitals also spread to Colonial America; Bellevue Hospital in New York City opened in 1736, first as a workhouse and then later as a hospital; Pennsylvania Hospital in Philadelphia opened in 1752, New York Hospital, now Weill Cornell Medical Center[40] in New York City opened in 1771, and Massachusetts General Hospital in Boston opened in 1811.
When the Vienna General Hospital opened in 1784 as the world's largest hospital, physicians acquired a new facility that gradually developed into one of the most important research centers.[41]
Another Enlightenment era charitable innovation was the dispensary; these would issue the poor with medicines free of charge. The London Dispensary opened its doors in 1696 as the first such clinic in the British Empire. The idea was slow to catch on until the 1770s,[42] when many such organisations began to appear, including the Public Dispensary of Edinburgh (1776), the Metropolitan Dispensary and Charitable Fund (1779) and the Finsbury Dispensary (1780). Dispensaries were also opened in New York 1771, Philadelphia 1786, and Boston 1796.[43]
The Royal Naval Hospital, Stonehouse, Plymouth, was a pioneer of hospital design in having "pavilions" to minimize the spread of infection. John Wesley visited in 1785, and commented "I never saw anything of the kind so complete; every part is so convenient, and so admirably neat. But there is nothing superfluous, and nothing purely ornamented, either within or without." This revolutionary design was made more widely known by John Howard, the philanthropist. In 1787 the French government sent two scholar administrators, Coulomb and Tenon, who had visited most of the hospitals in Europe.[44] They were impressed and the "pavilion" design was copied in France and throughout Europe.

English physician Thomas Percival (1740–1804) wrote a comprehensive system of medical conduct, Medical Ethics; or, a Code of Institutes and Precepts, Adapted to the Professional Conduct of Physicians and Surgeons (1803) that set the standard for many textbooks.[45] In the mid-19th century, hospitals and the medical profession became more professionalised, with a reorganisation of hospital management along more bureaucratic and administrative lines. The Apothecaries Act 1815 made it compulsory for medical students to practise for at least half a year at a hospital as part of their training.[46]
Florence Nightingale pioneered the modern profession of nursing during the Crimean War when she set an example of compassion, commitment to patient care and diligent and thoughtful hospital administration. The first official nurses' training programme, the Nightingale School for Nurses, was opened in 1860, with the mission of training nurses to work in hospitals, to work with the poor and to teach.[47] Nightingale was instrumental in reforming the nature of the hospital, by improving sanitation standards and changing the image of the hospital from a place the sick would go to die, to an institution devoted to recuperation and healing. She also emphasised the importance of statistical measurement for determining the success rate of a given intervention and pushed for administrative reform at hospitals.[48]
By the late 19th century, the modern hospital was beginning to take shape with a proliferation of a variety of public and private hospital systems. By the 1870s, hospitals had more than trebled their original average intake of 3,000 patients. In continental Europe the new hospitals generally were built and run from public funds. The National Health Service, the principal provider of health care in the United Kingdom, was founded in 1948. During the nineteenth century, the Second Viennese Medical School emerged with the contributions of physicians such as Carl Freiherr von Rokitansky, Josef Škoda, Ferdinand Ritter von Hebra, and Ignaz Philipp Semmelweis. Basic medical science expanded and specialisation advanced. Furthermore, the first dermatology, eye, as well as ear, nose, and throat clinics in the world were founded in Vienna, being considered as the birth of specialised medicine.[49]
|
|
The examples and perspective in this section deal primarily with the United States and do not represent a worldwide view of the subject. (August 2020)
|


By the late 19th and early 20th centuries, medical advancements such as anesthesia and sterile techniques that could make surgery less risky, and the availability of more advanced diagnostic devices such as X-rays, continued to make hospitals a more attractive option for treatment.[50]
Modern hospitals measure various efficiency metrics such as occupancy rates, the average length of stay, time to service, patient satisfaction, physician performance, patient readmission rate, inpatient mortality rate, and case mix index.[51]
In the United States, the number of hospitalizations grew to its peak in 1981 with 171 admissions per 1,000 Americans and 6,933 hospitals.[50] This trend subsequently reversed, with the rate of hospitalization falling by more than 10% and the number of US hospitals shrinking from 6,933 in 1981 to 5,534 in 2016.[52] Occupancy rates also dropped from 77% in 1980 to 60% in 2013.[53] Among the reasons for this are the increasing availability of more complex care elsewhere such as at home or the physicians' offices and also the less therapeutic and more life-threatening image of the hospitals in the eyes of the public.[50][54] In the US, a patient may sleep in a hospital bed, but be considered outpatient and "under observation" if not formally admitted.[55]
In the U.S., inpatient stays are covered under Medicare Part A, but a hospital might keep a patient under observation which is only covered under Medicare Part B, and subjects the patient to additional coinsurance costs.[55] In 2013, the Center for Medicare and Medicaid Services (CMS) introduced a "two-midnight" rule for inpatient admissions,[56] intended to reduce an increasing number of long-term "observation" stays being used for reimbursement.[55] This rule was later dropped in 2018.[56] In 2016 and 2017, healthcare reform and a continued decline in admissions resulted in US hospital-based healthcare systems performing poorly financially.[57] Microhospitals, with bed capacities of between eight and fifty, are expanding in the United States.[58] Similarly, freestanding emergency rooms, which transfer patients that require inpatient care to hospitals, were popularised in the 1970s[59] and have since expanded rapidly across the United States.[59]
The Catholic Church is the largest non-government provider of health careservices in the world.[60] It has around 18,000 clinics, 16,000 homes for the elderly and those with special needs, and 5,500 hospitals, with 65 percent of them located in developing countries.[61] In 2010, the Church's Pontifical Council for the Pastoral Care of Health Care Workers said that the Church manages 26% of the world's health care facilities.[62]

Modern hospitals derive funding from a variety of sources. They may be funded by private payment and health insurance or public expenditure, charitable donations.
In the United Kingdom, the National Health Service delivers health care to legal residents funded by the state "free at the point of delivery", and emergency care free to anyone regardless of nationality or status. Due to the need for hospitals to prioritise their limited resources, there is a tendency in countries with such systems for 'waiting lists' for non-crucial treatment, so those who can afford it may take out private health care to access treatment more quickly.[63]
In the United States, hospitals typically operate privately and in some cases on a for-profit basis, such as HCA Healthcare.[64] The list of procedures and their prices are billed with a chargemaster; however, these prices may be lower for health care obtained within healthcare networks.[65] Legislation requires hospitals to provide care to patients in life-threatening emergency situations regardless of the patient's ability to pay.[66] Privately funded hospitals which admit uninsured patients in emergency situations incur direct financial losses, such as in the aftermath of Hurricane Katrina.[64]
As the quality of health care has increasingly become an issue around the world, hospitals have increasingly had to pay serious attention to this matter. Independent external assessment of quality is one of the most powerful ways to assess this aspect of health care, and hospital accreditation is one means by which this is achieved. In many parts of the world such accreditation is sourced from other countries, a phenomenon known as international healthcare accreditation, by groups such as Accreditation Canada in Canada, the Joint Commission in the U.S., the Trent Accreditation Scheme in Great Britain, and the Haute Autorité de santé (HAS) in France. In England, hospitals are monitored by the Care Quality Commission. In 2020, they turned their attention to hospital food standards after seven patient deaths from listeria linked to pre-packaged sandwiches and salads in 2019, saying "Nutrition and hydration is part of a patient's recovery."[67]
The World Health Organization reported in 2011 that being admitted to a hospital was far riskier than flying. Globally, the chance of a patient being subject to a treatment error in a hospital was about 10%, and the chance of death resulting from an error was about one in 300. according to Liam Donaldson. 7% of hospitalised patients in developed countries, and 10% in developing countries, acquire at least one health care-associated infection. In the U.S., 1.7 million infections are acquired in hospital each year, leading to 100,000 deaths, figures much worse than in Europe where there were 4.5 million infections and 37,000 deaths.[68]
Modern hospital buildings are designed to minimise the effort of medical personnel and the possibility of contamination while maximising the efficiency of the whole system. Travel time for personnel within the hospital and the transportation of patients between units is facilitated and minimised. The building also should be built to accommodate heavy departments such as radiology and operating rooms while space for special wiring, plumbing, and waste disposal must be allowed for in the design.[69]
However, many hospitals, even those considered "modern", are the product of continual and often badly managed growth over decades or even centuries, with utilitarian new sections added on as needs and finances dictate. As a result, Dutch architectural historian Cor Wagenaar has called many hospitals:
"... built catastrophes, anonymous institutional complexes run by vast bureaucracies, and totally unfit for the purpose they have been designed for ... They are hardly ever functional, and instead of making patients feel at home, they produce stress and anxiety."[70]
Some newer hospitals now try to re-establish design that takes the patient's psychological needs into account, such as providing more fresh air, better views and more pleasant colour schemes. These ideas harken back to the late eighteenth century, when the concept of providing fresh air and access to the 'healing powers of nature' were first employed by hospital architects in improving their buildings.[70]
The research of British Medical Association is showing that good hospital design can reduce patient's recovery time. Exposure to daylight is effective in reducing depression.[71] Single-sex accommodation help ensure that patients are treated in privacy and with dignity. Exposure to nature and hospital gardens is also important – looking out windows improves patients' moods and reduces blood pressure and stress level. Open windows in patient rooms have also demonstrated some evidence of beneficial outcomes by improving airflow and increased microbial diversity.[72][73] Eliminating long corridors can reduce nurses' fatigue and stress.[74]
Another ongoing major development is the change from a ward-based system (where patients are accommodated in communal rooms, separated by movable partitions) to one in which they are accommodated in individual rooms. The ward-based system has been described as very efficient, especially for the medical staff, but is considered to be more stressful for patients and detrimental to their privacy. A major constraint on providing all patients with their own rooms is however found in the higher cost of building and operating such a hospital; this causes some hospitals to charge for private rooms.[75]
Although physicians were available in varying capacities in ancient Rome and Athens, the institution of a hospital dedicated to the care of the sick was a distinctly Christian innovation rooted in the monastic virtue and practise of hospitality. Arranged around the monastery were concentric rings of buildings in which the life and work of the monastic community was ordered. The outer ring of buildings served as a hostel in which travellers were received and boarded. The inner ring served as a place where the monastic community could care for the sick, the poor and the infirm. Monks were frequently familiar with the medicine available at that time, growing medicinal plants on the monastery grounds and applying remedies as indicated. As such, many of the practicing physicians of the Middle Ages were also clergy.
Another lasting advancement made during this time period was that of physician licensure. In 931 AD Caliph Al-Muqtadir learned that a patient had died in Baghdad as a result of a physician's error. Consequently, he ordered Sinan ibn Thabit to examine all those who practiced the art of healing. Of the 860 medical practitioners he examined, 160 failed. From that time on, licensing examinations were required and administered in various places. Licensing boards were set up under a government official called Muhtasib, or inspector general. The chief physician gave oral and practical examinations, and if the young physician was successful, the Muhtasib administered the Hippocratic Oath and issued a license to practice medicine.
|
This article needs additional citations for verification. (October 2007)
|
| Part of a series on |
| Accounting |
|---|
 |
Financial accounting is a branch of accounting concerned with the summary, analysis and reporting of financial transactions related to a business.[1] This involves the preparation of financial statements available for public use. Stockholders, suppliers, banks, employees, government agencies, business owners, and other stakeholders are examples of people interested in receiving such information for decision making purposes.
Financial accountancy is governed by both local and international accounting standards. Generally Accepted Accounting Principles (GAAP) is the standard framework of guidelines for financial accounting used in any given jurisdiction. It includes the standards, conventions and rules that accountants follow in recording and summarizing and in the preparation of financial statements.
On the other hand, International Financial Reporting Standards (IFRS) is a set of accounting standards stating how particular types of transactions and other events should be reported in financial statements. IFRS are issued by the International Accounting Standards Board (IASB).[2] With IFRS becoming more widespread on the international scene, consistency in financial reporting has become more prevalent between global organizations.
While financial accounting is used to prepare accounting information for people outside the organization or not involved in the day-to-day running of the company, managerial accounting provides accounting information to help managers make decisions to manage the business.
Financial accounting and financial reporting are often used as synonyms.
1. According to International Financial Reporting Standards: the objective of financial reporting is:
To provide financial information that is useful to existing and potential investors, lenders and other creditors in making decisions about providing resources to the reporting entity.[3]
2. According to the European Accounting Association:
Capital maintenance is a competing objective of financial reporting.[4]
Financial accounting is the preparation of financial statements that can be consumed by the public and the relevant stakeholders. Financial information would be useful to users if such qualitative characteristics are present. When producing financial statements, the following must comply: Fundamental Qualitative Characteristics:
Enhancing Qualitative Characteristics:
The statement of cash flows considers the inputs and outputs in concrete cash within a stated period. The general template of a cash flow statement is as follows: Cash Inflow - Cash Outflow + Opening Balance = Closing Balance
Example 1: in the beginning of September, Ellen started out with $5 in her bank account. During that same month, Ellen borrowed $20 from Tom. At the end of the month, Ellen bought a pair of shoes for $7. Ellen's cash flow statement for the month of September looks like this:
Example 2: in the beginning of June, WikiTables, a company that buys and resells tables, sold 2 tables. They'd originally bought the tables for $25 each, and sold them at a price of $50 per table. The first table was paid out in cash however the second one was bought in credit terms. WikiTables' cash flow statement for the month of June looks like this:
Important: the cash flow statement only considers the exchange of actual cash, and ignores what the person in question owes or is owed.
The statement of profit or income statement represents the changes in value of a company's accounts over a set period (most commonly one fiscal year), and may compare the changes to changes in the same accounts over the previous period. All changes are summarized on the "bottom line" as net income, often reported as "net loss" when income is less than zero.
The net profit or loss is determined by:
Sales (revenue)
– selling, general, administrative expenses (SGA)
– depreciation/ amortization
= earnings before interest and taxes (EBIT)
– interest and tax expenses
= profit/loss
The balance sheet is the financial statement showing a firm's assets, liabilities and equity (capital) at a set point in time, usually the end of the fiscal year reported on the accompanying income statement. The total assets always equal the total combined liabilities and equity. This statement best demonstrates the basic accounting equation:
Assets = Liabilities + Equity
The statement can be used to help show the financial position of a company because liability accounts are external claims on the firm's assets while equity accounts are internal claims on the firm's assets.
Accounting standards often set out a general format that companies are expected to follow when presenting their balance sheets. International Financial Reporting Standards (IFRS) normally require that companies report current assets and liabilities separately from non-current amounts.[5][6] A GAAP-compliant balance sheet must list assets and liabilities based on decreasing liquidity, from most liquid to least liquid. As a result, current assets/liabilities are listed first followed by non-current assets/liabilities. However, an IFRS-compliant balance sheet must list assets/liabilities based on increasing liquidity, from least liquid to most liquid. As a result, non-current assets/liabilities are listed first followed by current assets/liabilities.[7]
Current assets are the most liquid assets of a firm, which are expected to be realized within a 12-month period. Current assets include:
Non-current assets include fixed or long-term assets and intangible assets:
Liabilities include:
Owner's equity, sometimes referred to as net assets, is represented differently depending on the type of business ownership. Business ownership can be in the form of a sole proprietorship, partnership, or a corporation. For a corporation, the owner's equity portion usually shows common stock, and retained earnings (earnings kept in the company). Retained earnings come from the retained earnings statement, prepared prior to the balance sheet.[8]
This statement is additional to the three main statements described above. It shows how the distribution of income and transfer of dividends affects the wealth of shareholders in the company. The concept of retained earnings means profits of previous years that are accumulated till current period. Basic proforma for this statement is as follows:
Retained earnings at the beginning of period
+ Net Income for the period
- Dividends
= Retained earnings at the end of period.[9]
One of the basic principles in accounting is "The Measuring Unit principle":
The unit of measure in accounting shall be the base money unit of the most relevant currency. This principle also assumes the unit of measure is stable; that is, changes in its general purchasing power are not considered sufficiently important to require adjustments to the basic financial statements."[10]
Historical Cost Accounting, i.e., financial capital maintenance in nominal monetary units, is based on the stable measuring unit assumption under which accountants simply assume that money, the monetary unit of measure, is perfectly stable in real value for the purpose of measuring (1) monetary items not inflation-indexed daily in terms of the Daily CPI and (2) constant real value non-monetary items not updated daily in terms of the Daily CPI during low and high inflation and deflation.
The stable monetary unit assumption is not applied during hyperinflation. IFRS requires entities to implement capital maintenance in units of constant purchasing power in terms of IAS 29 Financial Reporting in Hyperinflationary Economies.
Financial accountants produce financial statements based on the accounting standards in a given jurisdiction. These standards may be the Generally Accepted Accounting Principles of a respective country, which are typically issued by a national standard setter, or International Financial Reporting Standards (IFRS), which are issued by the International Accounting Standards Board (IASB).
Financial accounting serves the following purposes:
The accounting equation (Assets = Liabilities + Owners' Equity) and financial statements are the main topics of financial accounting.
The trial balance, which is usually prepared using the double-entry accounting system, forms the basis for preparing the financial statements. All the figures in the trial balance are rearranged to prepare a profit & loss statement and balance sheet. Accounting standards determine the format for these accounts (SSAP, FRS, IFRS). Financial statements display the income and expenditure for the company and a summary of the assets, liabilities, and shareholders' or owners' equity of the company on the date to which the accounts were prepared.
Asset, expense, and dividend accounts have normal debit balances (i.e., debiting these types of accounts increases them).
Liability, revenue, and equity accounts have normal credit balances (i.e., crediting these types of accounts increases them).
0 = Dr Assets Cr Owners' Equity Cr Liabilities . _____________________________/\____________________________ . . / Cr Retained Earnings (profit) Cr Common Stock \ . . _________________/\_______________________________ . . . / Dr Expenses Cr Beginning Retained Earnings \ . . . Dr Dividends Cr Revenue . . \________________________/ \______________________________________________________/ increased by debits increased by credits Crediting a credit Thus -------------------------> account increases its absolute value (balance) Debiting a debit Debiting a credit Thus -------------------------> account decreases its absolute value (balance) Crediting a debit
When the same thing is done to an account as its normal balance it increases; when the opposite is done, it will decrease. Much like signs in math: two positive numbers are added and two negative numbers are also added. It is only when there is one positive and one negative (opposites) that you will subtract.
However, there are instances of accounts, known as contra-accounts, which have a normal balance opposite that listed above. Examples include:
Many professional accountancy qualifications cover the field of financial accountancy, including Certified Public Accountant CPA, Chartered Accountant (CA or other national designations, American Institute of Certified Public Accountants AICPA and Chartered Certified Accountant (ACCA).